National Communications
The National Medical Association is the 125+-year-old voice of African American physicians in America. In recent years, I’ve provided communications planning, editorial services, media relations and other support in collaboration with colleagues at Think Inspired Marketing. My efforts helped extend its reach, enhance its profile and amplify its voice.
NMA Media Report 1
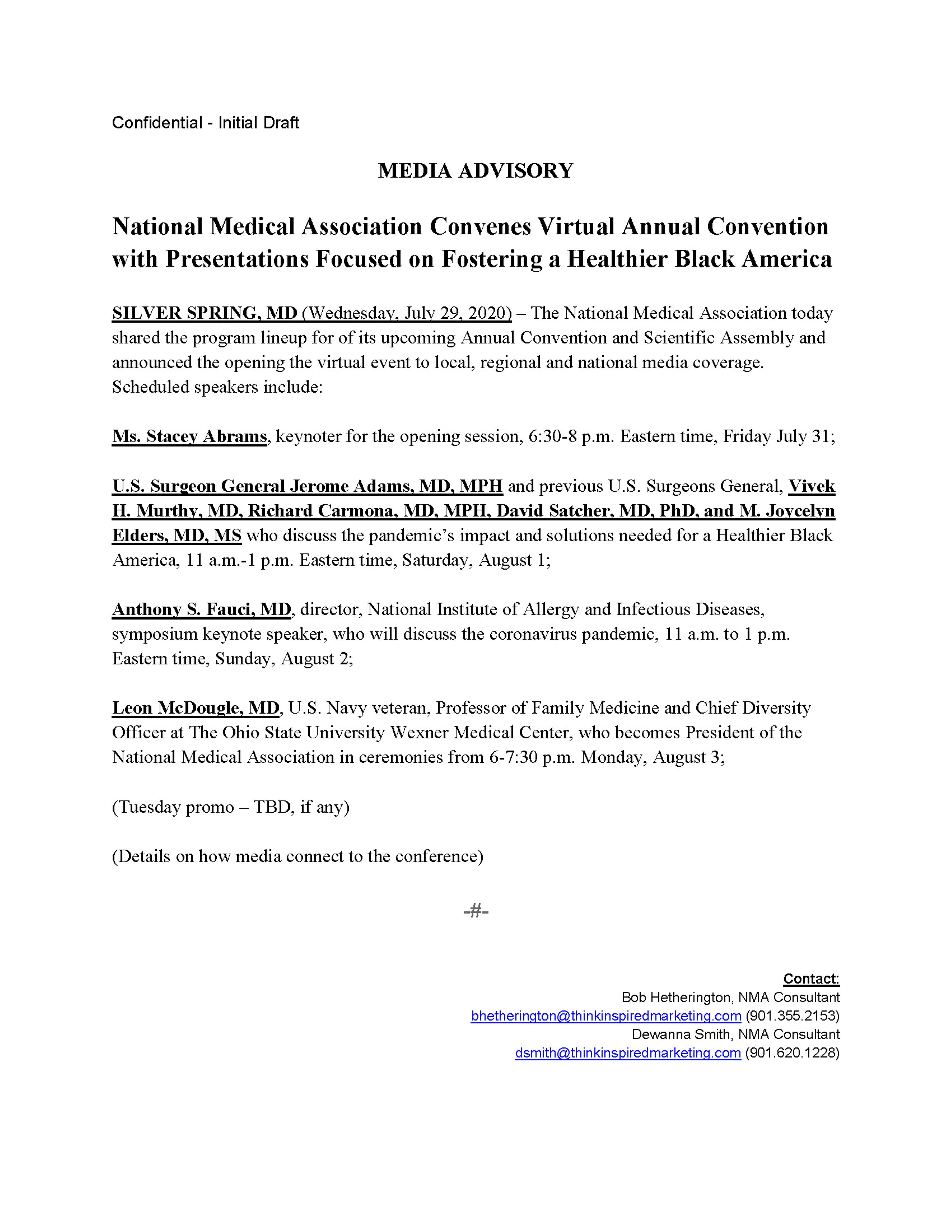
The pre-event media advisory was distributed to hundreds of media outlets across America.
The advisory was shared and personally pitched to key editors, medical writers, reporters and producers at:
The Associated Press in Washington, D.C.
Reuters in Washington, D.C.
National Public Radio in Washington, D.C.
Reporters with The New York Times in New York
Senior producer at MSNBC who works with Joy Reid, other anchors
CNN and ABC
The advisory was personally shared with major metro newspapers which serve large numbers of African American readers. They include:
The Advocate in Baton Rouge
Atlanta Journal and Constitution
Baltimore Sun
Birmingham News
Clarion Ledger, Jackson, Mississippi
Cleveland Plain Dealer
Detroit Free Press News
Memphis Commercial Appeal
Miami Herald
Montgomery Advertiser
New Orleans Times Picyune
Northwest Indiana Times
Philadelphia Inquirer
Wilmington DE News Journal
Our outreach was successful. For example, Pulitzer Prize winning reporter Susan Snyder at the Philadelphia Inquirer reached out to us on both Friday and Saturday for assistance in accessing the event so she could monitor remarks but especially those by Dr. Anthony Fauci.
In addition, the media advisory went out to more than 300 African American owned and operated dailies, weeklies and monthly publications in 38 states. (List below)
The media advisory about the annual meeting went out to more than 210 African America owned and oriented radio stations across the country and more than two dozen television stations. (List below)
Previously shared clips and links to more than three dozens postings or publications.
For example, National Association of Diversity Officer of Higher Education
https://twitter.com/nadohe_?lang=en
For example, Black Chronicle (5,000 to 7,500 daily)
Confidential Draft
Think Inspired for National Medical Association
Earned Media Roundup
August 31, 2020
Here is a recap of pro-active media relations activities, distribution report on the pre-event media advisory and a sampling of NMA annual meeting related media coverage.
Columbus, Ohio coverage
Public Radio – The Ohio State University
https://www.newsbreak.com/amp/samsung-daily/n/0PqDDpDV
https://wcpn.ideastream.org/news/ohio-state-professor-takes-helm-at-national-medical-association
Columbus CEO
https://www.newsbreak.com/amp/samsung-daily/n/0WgVu8Hj
WSKU FM – radio interview
https://www.wksu.org/post/ohio-state-professor-takes-helm-national-medical-association#stream/0
Columbus Dispatch – McDougle Guest Column
Memphis Commercial Appeal – McDougle Guest Column
Confidential Draft
Guest Column—Columbus Dispatch
Columbus, Ohio – July 30, 2020
By Leon McDougle, MD, MPH
As a family physician in Columbus, Ohio, when someone has chest pain with exertion that might be caused by a blockage of a heart artery, I order a cardiac stress test. The coronavirus pandemic is a stress test for African Americans and people of color across the USA today.
As the incoming president of the National Medical Association, I assure you the results of this COVID-19 stress test call for immediate, life-preserving interventions, as health disparities, a legacy of chattel slavery, continue across our nation with no end in sight.
In April, based on the earliest available data, Cato T. Laurencin, MD, PhD, reported on the disproportionate impact of the novel coronavirus on black citizens of Connecticut in a peer-reviewed journal. Dr. Laurencin, a distinguished professor of orthopedic surgery at the University of Connecticut, noted their vulnerability because they already are disproportionately affected by poverty, limited health care access and health-related conditions, including heart disease, diabetes, kidney disease and respiratory illness, among others.
“While the virus does not discriminate,” he noted, “America’s history of discrimination creates potential longer-term scenarios akin to our experience with HIV, influenza, and other infectious diseases in Black and Brown people.”
Our experience with COVID-19 since then has proven his assessment was prescient.
Over the past 125 years, the National Medical Association has served as a collective voice for African American physicians and their patients.
In the year ahead, our organization will work with others to address disparities in health access and outcomes and advance health equity, so all Americans have a fair, just opportunity to be as healthy as possible.
The NMA will work to accelerate a broader, more equitable and just response to the nation’s COVID-19 crisis. The latest data show rates of infection and death among African Americans are disproportionately high and related to pre-existing health disparities, structural impediments, and inadequate strategies to address the unequal health and healthcare in the African American community specifically and in communities of color overall.
I will soon convene a National Medical Association COVID-19 Commission which will include experts on vaccines, therapeutics, policy, practice, access and prevention. We will learn from this bitter experience. And we will work to have our communities and our country better prepared and better equipped to respond to the next health crisis.
If the United States government can allocate tax breaks and benefits for the wealthy and corporations that will cost $2.3 trillion over 10 years as it did in 2018, then to start, it is time for an investment of similar magnitude in institutions advancing health equity. These include more than 100 historically black colleges and universities. These include Meharry Medical College in Nashville, Howard University College of Medicine in Washington, D.C., Morehouse School of Medicine in Atlanta and Charles R. Drew Medical School in Los Angeles and the W. Montague Cobb/National Medical Association Health Institute.
Under my leadership, NMA will continue working to create broader access and foster greater diversity among individuals pursuing careers in health-related professions. America faces a physician shortage of 40,000 to 120,000 over the next decade in both primary and specialty care. The proportion of med students who identified as African American rose from 5.6 percent in 1980 to 7.1 percent in 2018. Even so, that is still well short of the 13.4 percent of Americans who are black.
Additionally, NMA will amplify efforts to promote social justice, changes to reduce racism-driven deaths from police-involved violence, to bring an end to the mass incarceration of African Americans and to abolish the inequitably applied death penalty.
Hurricane Katrina in 2005 and the novel coronavirus pandemic this year revealed infrastructure failures which have worsened health disparities in black neighborhoods and resulted in the untimely deaths of black people and people of color.
Hurricane Katrina revealed cracks in the levees. The novel coronavirus revealed a broken public health and emergency response infrastructures in desperate need of repair. In both cases, those failures put lives in jeopardy and caused unnecessary deaths.
As President of the NMA and a representative of Black physicians nationwide, I am prepared to lead with one voice. Our nation can and must do better.
Leon McDougle, MD, MPH, is a U.S. Navy veteran, a Professor of Family Medicine and Chief Diversity Officer at The Ohio State University Wexner Medical Center and President of the National Medical Association.
Column: Amid COVID-19 pandemic, national Black physicians group addresses disparities
Leon McDougle, M.D., Guest columnist
As a family physician in Columbus, when someone has chest pain with exertion that might be caused by a blockage of a heart artery, I order a cardiac stress test. The coronavirus pandemic is a stress test for African Americans and people of color across the USA today.
As the new president of the National Medical Association, I assure you the results of this COVID-19 stress test call for immediate, life-preserving interventions, as health disparities, a legacy of chattel slavery, continue across our nation with no end in sight.
In April, based on the earliest available data, Cato T. Laurencin, M.D., Ph.D., reported on the disproportionate impact of the novel coronavirus on black citizens of Connecticut in a peer-reviewed journal. Laurencin, a distinguished professor of orthopedic surgery at the University of Connecticut, noted their vulnerability because they already are disproportionately affected by poverty, limited health care access and health-related conditions, including heart disease, diabetes, kidney disease and respiratory illness.
“While the virus does not discriminate,” he noted, “America’s history of discrimination creates potential longer-term scenarios akin to our experience with HIV, influenza, and other infectious diseases in Black and brown people.”
Our experience with COVID-19 since then has proved his assessment was prescient.
In the past 125 years, the National Medical Association has served as a collective voice for African American physicians and their patients.
In the year ahead, our organization will work with others to address disparities in health access and outcomes and advance health equity, so all Americans have a fair, just opportunity to be as healthy as possible.
The NMA will work to accelerate a broader, more equitable and just response to the nation’s COVID-19 crisis. The latest data show rates of infection and death among African Americans are disproportionately high and related to preexisting health disparities, structural impediments and inadequate strategies to address the unequal health and health care in the African American community specifically and in communities of color overall.
I will soon convene a National Medical Association COVID-19 Commission that will include experts on vaccines, therapeutics, policy, practice, access and prevention. We will learn from this bitter experience. And we will work to have our communities and our country better prepared and better equipped to respond to the next health crisis.
If the United States government can allocate tax breaks and benefits for the wealthy and corporations that will cost $2.3 trillion over 10 years as it did in 2018, then it is time for an investment of similar magnitude in institutions advancing health equity. These include more than 100 historically black colleges and universities such as Meharry Medical College in Nashville; Howard University College of Medicine in Washington, D.C.; Morehouse School of Medicine in Atlanta; Charles R. Drew Medical School in Los Angeles; and the W. Montague Cobb/National Medical Association Health Institute.
Under my leadership, NMA will continue working to create broader access and foster greater diversity among individuals pursuing careers in health-related professions. America faces a physician shortage of 40,000 to 120,000 in the next decade in both primary and specialty care. The proportion of med students who identified as African American rose from 5.6% in 1980 to 7.1% in 2018. Even so, that is still well short of the 13.4% of Americans who are black.
Additionally, NMA will amplify efforts to promote social justice, seek changes to reduce racism-driven deaths from police-involved violence, bring an end to the mass incarceration of African Americans and abolish the inequitably applied death penalty.
Hurricane Katrina in 2005 and the novel coronavirus pandemic this year revealed infrastructure failures that have worsened health disparities in Black neighborhoods and resulted in the untimely deaths of Black people and people of color.
Hurricane Katrina revealed cracks in the levees. The novel coronavirus revealed broken public health and emergency response infrastructures in desperate need of repair. In both cases, those failures put lives in jeopardy and caused unnecessary deaths.
As president of the NMA and a representative of Black physicians nationwide, I am prepared to lead with one voice. Our nation can and must do better.
Leon McDougle, M.D., MPH, is a U.S. Navy veteran, a professor of family medicine and chief diversity officer at The Ohio State University Wexner Medical Center, and president of the National Medical Association.
National Medical Association pledges to lead charge in social justice, COVID-19 response | Opinion
The novel coronavirus revealed a broken public health and emergency response infrastructures in desperate need of repair.
Leon McDougle, MD, MPH, Guest Columnist
As a family physician in Columbus, Ohio, when someone has chest pain with exertion that might be caused by a blockage of a heart artery, I order a cardiac stress test.
The coronavirus pandemic is a stress test for African Americans and people of color across the USA today.
As the incoming president of the National Medical Association, I assure you the results of this COVID-19 stress test call for immediate, life-preserving interventions, as health disparities, a legacy of chattel slavery, continue across our nation with no end in sight.
In April, based on the earliest available data, Cato T. Laurencin, MD, PhD, reported on the disproportionate impact of the novel coronavirus on Black citizens of Connecticut in a peer-reviewed journal.
Dr. Laurencin, a distinguished professor of orthopedic surgery at the University of Connecticut, noted their vulnerability because they already are disproportionately affected by poverty, limited health care access and health-related conditions, including heart disease, diabetes, kidney disease and respiratory illness, among others.
“While the virus does not discriminate,” he noted, “America’s history of discrimination creates potential longer-term scenarios akin to our experience with HIV, influenza, and other infectious diseases in Black and Brown people.”
Our experience with COVID-19 has proven his assessment was prescient
Over the past 125 years, the National Medical Association has served as a collective voice for African American physicians and their patients.
In the year ahead, our organization will work with others to address disparities in health access and outcomes and advance health equity, so all Americans have a fair, just opportunity to be as healthy as possible.
The NMA will work to accelerate a broader, more equitable and just response to the nation’s COVID-19 crisis. The latest data show rates of infection and death among African Americans are disproportionately high and related to pre-existing health disparities, structural impediments, and inadequate strategies to address the unequal health and healthcare in the African American community specifically and in communities of color overall.
I will soon convene a National Medical Association COVID-19 Commission which will include experts on vaccines, therapeutics, policy, practice, access and prevention. We will learn from this bitter experience. And we will work to have our communities and our country better prepared and better equipped to respond to the next health crisis.
If the United States government can allocate tax breaks and benefits for the wealthy and corporations that will cost $2.3 trillion over 10 years as it did in 2018, then to start, it is time for an investment of similar magnitude in institutions advancing health equity. These include more than 100 historically Black colleges and universities.
These include Meharry Medical College in Nashville, Howard University College of Medicine in Washington, D.C., Morehouse School of Medicine in Atlanta and Charles R. Drew Medical School in Los Angeles and the W. Montague Cobb/National Medical Association Health Institute.
Under my leadership, NMA will continue working to create broader access and foster greater diversity among individuals pursuing careers in health-related professions. America faces a physician shortage of 40,000 to 120,000 over the next decade in both primary and specialty care.
The proportion of med students who identified as African American rose from 5.6% in 1980 to 7.1% in 2018. Even so, that is still well short of the 13.4 percent of Americans who are Black.
Additionally, NMA will amplify efforts to promote social justice, changes to reduce racism-driven deaths from police-involved violence, to bring an end to the mass incarceration of African Americans and to abolish the inequitably applied death penalty.
Hurricane Katrina in 2005 and the novel coronavirus pandemic this year revealed infrastructure failures which have worsened health disparities in Black neighborhoods and resulted in the untimely deaths of Black people and people of color.
Hurricane Katrina revealed cracks in the levees. The novel coronavirus revealed a broken public health and emergency response infrastructures in desperate need of repair. In both cases, those failures put lives in jeopardy and caused unnecessary deaths.
As President of the NMA and a representative of Black physicians nationwide, I am prepared to lead with one voice. Our nation can and must do better.
Leon McDougle, MD, MPH, is a U.S. Navy veteran, a Professor of Family Medicine and Chief Diversity Officer at The Ohio State University Wexner Medical Center and President of the National Medical Association.